A patient K., 37 years old, complained of an aesthetic defect of the anterior teeth crowns 1.1, 2.1, 2.2. The teeth had been treated endodontally many times before, but the patient said that the inflammation process used to be severe from time to time. The patient smokes up to 20 cigarettes a day. Three months ago, direct implantation to the tooth socket had taken place 1.2, in the postoperative period a stagnant wound process was observed, the wound borders expanded slightly, but it did not influence the implant integration.
At the oral cavity examination, a temporary construction in the area of the teeth is seen 1.1, 2.1, 2.2, Bio3 implant 3.8/13 is placed where the missing tooth was (1.2). There are no signs of chronic periodontitis exacerbation of the teeth in the alveolar process area, the gum biotype is thin, the smile line is high (Fig. 1).

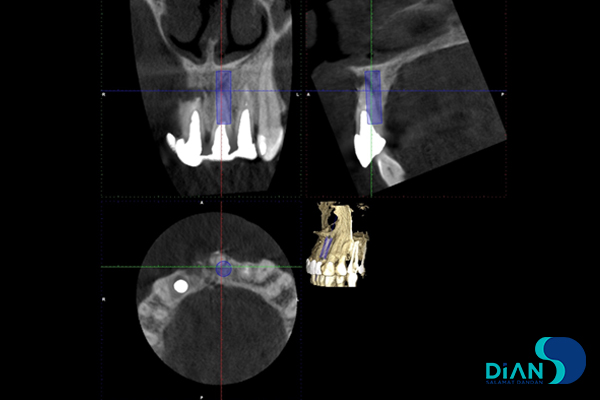
CBCT shows the signs of apical periodontitis in the teeth 1.1, 2.1, as well as root fractures that cannot be restored. The vestibular plate of the tooth socket 2.1 is not seen (Fig. 2).
Taking into account all the peculiarities of the clinical case, extraction of the tooth with one-stage implantation and the vestibular wall defect grafting in the socket with a cortical-spongious bone graft from the genian lower jaw was offered. This technique was chosen because of the high risk of the implanted material loss at using GBR method for this patient, which is connected with her harmful habit.
The surgery processes
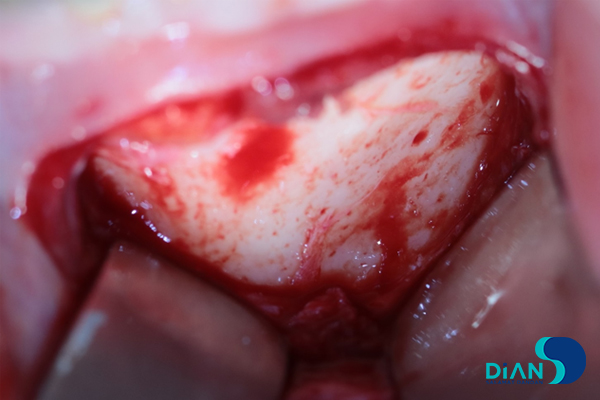
Under local anesthesia with 4% Ultracain solution, after processing of the surgical area with Betadine solution a cut of the lower lip mucous membrane at the level of the teeth 3.1. 3.2. 3.3 was made. The tissues were cut in layers by sharp dissection to the bone with m. mentalis crossing, the vestibular surface of the genian lower jaw was skeletonized with an elevator (Fig. 3).
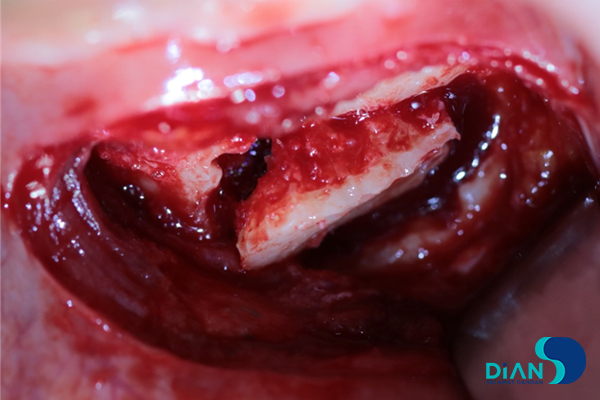
Moving 5-6 mm down from the top of the lower incisor roots, a 1.0×0.5 cm cut of the cortical plate was made. The fragment was separated from the lower jaw with an osseotome and placed into NaCl 0.9% sterile solution (Fig. 4).
A homeostatic tube was placed on the spot where the bone defect appeared. The wound was closed up tightly in layers, with preliminary m. mentalis stitching, a compression band was put (Fig. 5).
The next step was making a cut through the gingival space in the area of the teeth (Fig. 6).

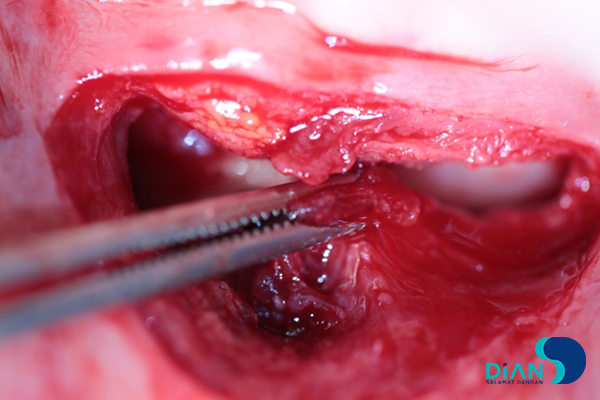
The vestibular surface of the maxillary alveolar process was skeletonized with an elevator, the tooth 1.1., 2.1., 2.2. was extracted (Fig. 7).
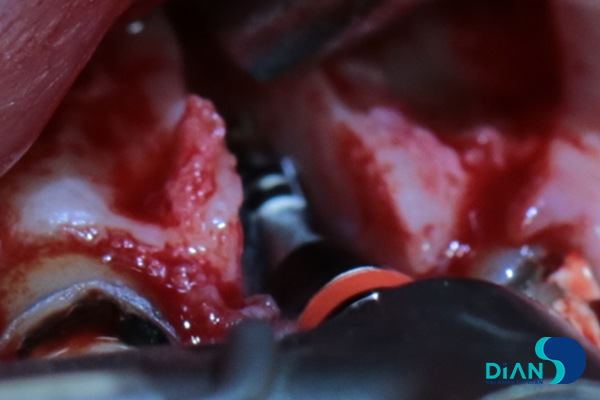
A thin and movable anterior wall of the extracted tooth socket is seen (Fig. 8), the latter was removed, and the defect borders were smoothed with a bur. The socket was examined, curettage and thorough rinsing of the wound with an antiseptic solution were done.

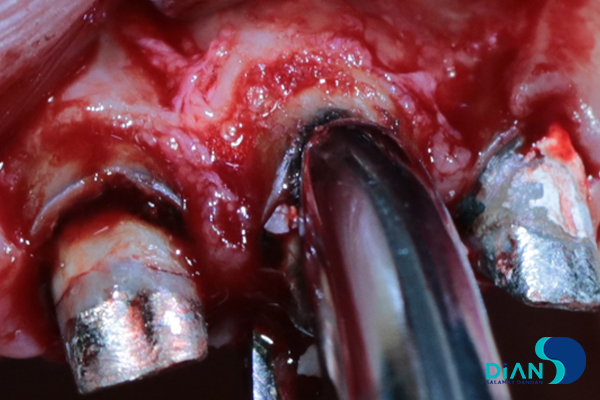
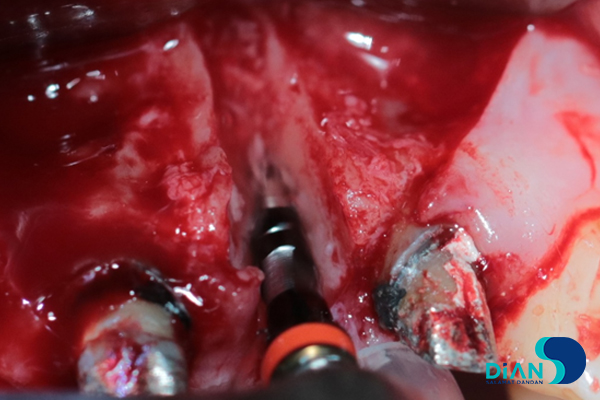
By means of a range of osseotomies for the palatal socket wall, according to the Bio3 implants protocols, an implant site was formed (Fig. 9-13).
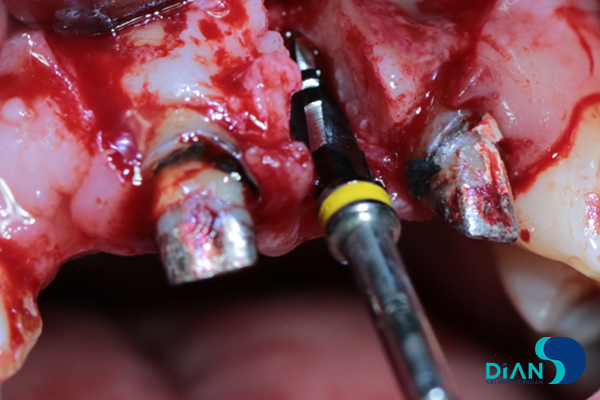
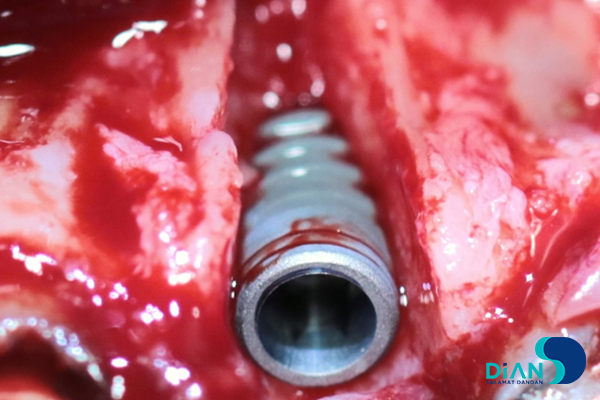
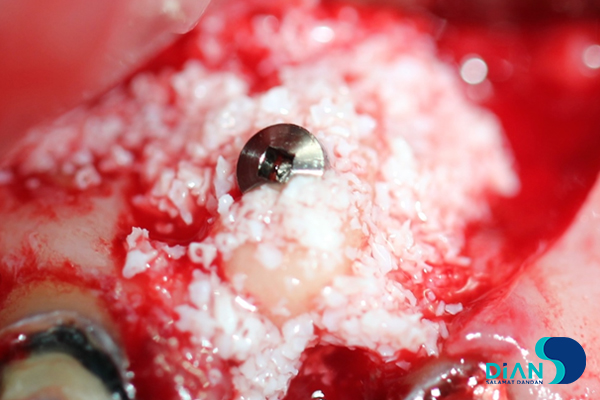
The implant Bio3 Progressive 3.8/13 was placed and fixed with 35-40 N (Fig. 14).
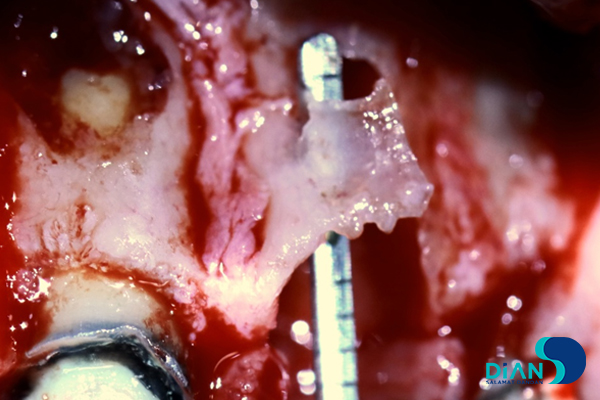
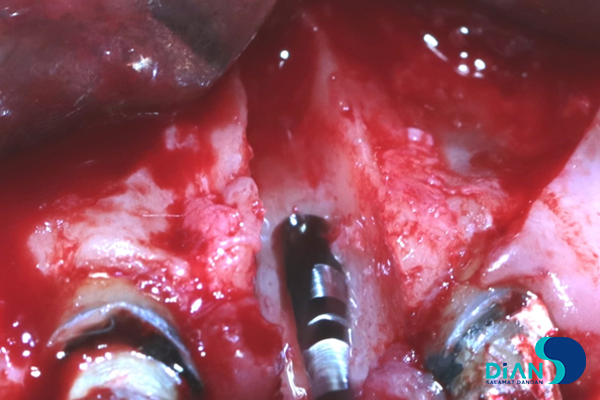
The bone block prepared beforehand was fitted to the defect contours and fixed there with a titanium screw to the basis of the interalveolar septum of the teeth 2.1 and 2.2 (Fig. 15).

The surface of the graft was covered with a synthetic osteoplastic material and 3 layers of PRF-membranes (Fig. 16-17).

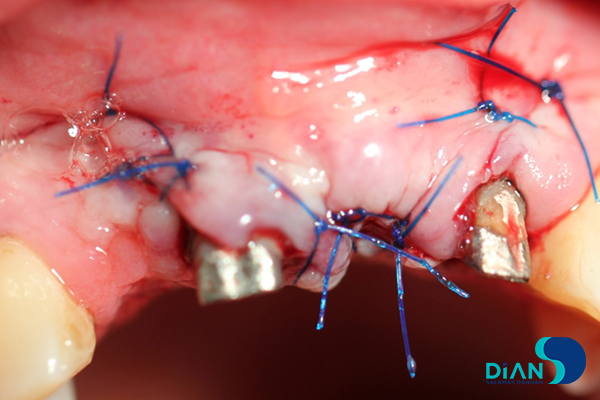
The flap was put to its place, the wound was closed up tightly with nylon thread (Fig. 18).
The check spot-film radiography was in the area of the placed implant was done (Fig. 19).

For the postoperative period anesthetic and antibacterial therapy was prescribed according to the generally accepted schemes.